Understanding Type 1 Diabetes: Causes, Symptoms, and Management
Type 1 diabetes, often diagnosed in children, teens, and young adults, is a chronic condition where the body’s immune system attacks the insulin-producing beta cells in the pancreas. Unlike Type 2 diabetes, Type 1 diabetes has no relation to lifestyle factors and is typically considered an autoimmune condition. While there’s currently no cure, advancements in treatment and technology have made it increasingly manageable, allowing those diagnosed to live full, active lives.
In this article, we’ll explore what Type 1 diabetes is, what causes it, how to recognize its symptoms, and the essential steps for effective management.
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune disease. The immune system, which typically defends the body against harmful invaders, mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Insulin is a hormone essential for regulating blood sugar levels and allowing glucose to enter cells for energy. Without insulin, blood sugar levels rise dangerously high, and glucose cannot enter the cells.
As a result, people with Type 1 diabetes require lifelong insulin therapy. The condition typically appears in childhood or early adulthood, although it can develop at any age.
Causes of Type 1 Diabetes
The exact cause of Type 1 diabetes remains unknown, though researchers believe a combination of genetic and environmental factors contribute to its onset. Here are some factors thought to play a role:
- Genetics: Certain genes may increase susceptibility to Type 1 diabetes. If you have a family history of the condition, your risk might be slightly higher, though it’s still uncommon.
- Autoimmune Triggers: In some cases, environmental factors like viral infections may trigger the immune system to attack the pancreas. These infections are believed to initiate the autoimmune response that leads to Type 1 diabetes.
- Environmental Factors: Exposure to toxins or certain dietary factors early in life may play a role, though evidence on specific environmental triggers is still inconclusive.
Unlike Type 2 diabetes, lifestyle factors like diet and exercise do not contribute to the development of Type 1 diabetes.
Symptoms of Type 1 Diabetes
Type 1 diabetes symptoms can come on suddenly and are often severe. If left untreated, they can lead to a condition called diabetic ketoacidosis (DKA), a dangerous buildup of acids in the blood. Key symptoms of Type 1 diabetes include:
- Frequent urination: High blood sugar levels lead to increased urination as the body attempts to remove excess glucose.
- Increased thirst: Frequent urination leads to dehydration, resulting in increased thirst.
- Unintended weight loss: The body begins to break down muscle and fat for energy, leading to weight loss.
- Extreme hunger: Without insulin, cells can’t access glucose, leading to persistent hunger.
- Fatigue: Without glucose for energy, the body often feels tired or weak.
- Blurred vision: High blood sugar levels can cause fluid to shift in the eye, affecting vision.
- Slow-healing sores or frequent infections: High blood sugar can impair immune response, leading to infections or slow healing.
If you experience these symptoms, it’s essential to seek medical attention, as early diagnosis and treatment can prevent complications.
Diagnosing Type 1 Diabetes
Diagnosing Type 1 diabetes involves several tests to check blood glucose levels and confirm the autoimmune nature of the condition:
- Blood Glucose Test: A simple blood test measures fasting and non-fasting glucose levels to determine if they are abnormally high.
- HbA1c Test: This test shows average blood sugar levels over the past 2-3 months, providing an indication of overall blood sugar control.
- Autoantibody Tests: Since Type 1 diabetes is an autoimmune condition, specific antibodies in the blood can indicate the immune system is attacking pancreatic cells.
- C-Peptide Test: This test measures how much insulin your pancreas is producing. A low level of C-peptide indicates low or no insulin production, which is typical in Type 1 diabetes.
Managing Type 1 Diabetes
Effective management of Type 1 diabetes involves maintaining stable blood glucose levels through a combination of insulin therapy, diet, exercise, and monitoring. Here’s how:
1. Insulin Therapy
Insulin therapy is essential for people with Type 1 diabetes since their bodies can’t produce insulin. There are several forms of insulin, categorized by how quickly they start to work, how long they last, and how they are delivered:
- Rapid-acting Insulin: Used before meals to cover spikes in blood sugar.
- Short-acting Insulin: Also used around mealtime but has a slightly longer duration.
- Intermediate-acting Insulin: Often taken twice a day to help with blood sugar levels between meals.
- Long-acting Insulin: Provides a baseline level of insulin for up to 24 hours.
Insulin can be administered through injections or an insulin pump, which delivers insulin throughout the day.
2. Continuous Glucose Monitoring (CGM)
Continuous glucose monitors provide real-time data on blood sugar levels, alerting the user to any significant changes. CGM devices reduce the need for frequent finger pricks, making blood sugar monitoring more manageable and providing more precise data for insulin dosing.
3. Dietary Choices
People with Type 1 diabetes don’t have a “one-size-fits-all” diet, but balanced nutrition is essential. Carbohydrates have the most significant impact on blood sugar, so counting carbs is critical to managing diabetes. Key dietary tips include:
- Balanced meals: Include a mix of proteins, healthy fats, and complex carbs to help maintain stable blood sugar.
- Fiber-rich foods: Fiber slows the absorption of carbs, helping prevent spikes in blood sugar.
- Limit sugary foods: Sugary foods can cause rapid increases in blood sugar levels, making management difficult.
A registered dietitian or certified diabetes educator can help create a meal plan tailored to individual needs and lifestyle.
4. Regular Exercise
Exercise can improve insulin sensitivity, meaning the body uses insulin more effectively, leading to better blood sugar control. However, for people with Type 1 diabetes, exercise can have a complex impact on blood sugar levels. Here’s what to consider:
- Monitor blood sugar: Check blood sugar levels before, during, and after exercise.
- Carry snacks: Keep fast-acting carbohydrates like glucose tablets or juice on hand in case of low blood sugar.
- Stay hydrated: Dehydration can raise blood sugar levels, so drink plenty of water.
Working with a healthcare provider can help you develop an exercise plan that fits your routine and helps keep blood sugar levels stable.
5. Stress Management
Stress can raise blood sugar levels and affect diabetes management. Practices such as mindfulness, meditation, yoga, and deep breathing can help reduce stress and improve overall well-being.
6. Education and Support
Managing Type 1 diabetes can be challenging, both physically and emotionally. Many healthcare providers offer educational programs and support groups to help people with diabetes and their families. Peer support, whether online or in-person, can also provide emotional support and practical tips for daily management.
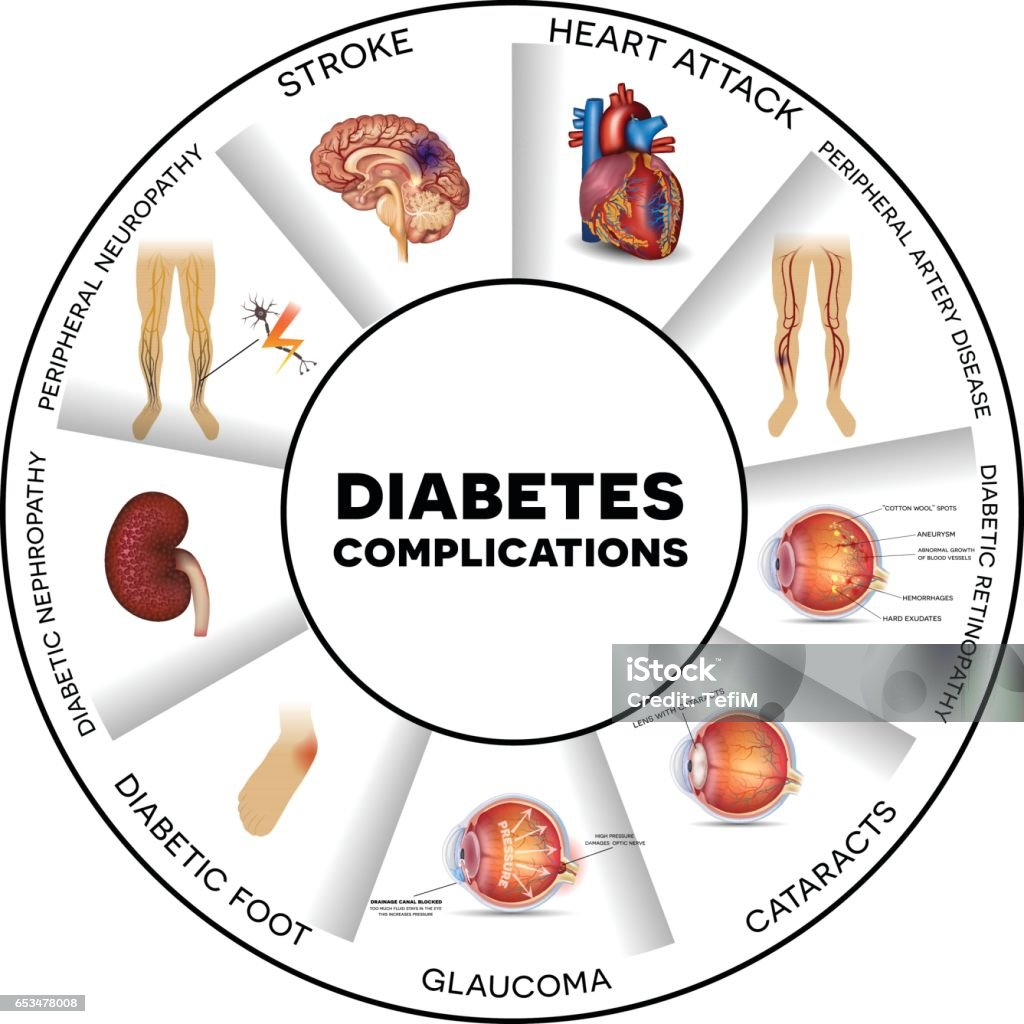
Complications of Type 1 Diabetes
Without proper management, Type 1 diabetes can lead to serious complications. Long-term complications include:
- Heart Disease: Uncontrolled diabetes increases the risk of heart disease and stroke.
- Kidney Damage: High blood sugar levels can lead to kidney damage and, in severe cases, kidney failure.
- Nerve Damage: Diabetes can lead to neuropathy, causing pain, tingling, or numbness, especially in the hands and feet.
- Eye Damage: Diabetes is a leading cause of blindness due to conditions like diabetic retinopathy.
Maintaining stable blood sugar levels and regular check-ups can prevent or delay these complications.
The Future of Type 1 Diabetes Management
Research is ongoing to improve Type 1 diabetes management. Innovations like artificial pancreas systems, new insulin formulations, and advancements in CGM technology offer hope for better quality of life. Stem cell research and immunotherapy also hold promise for potential treatments that could one day lead to a cure.
Final Thoughts
Type 1 diabetes requires diligent management, but with the right approach, people can live full, active lives. By combining insulin therapy, diet, exercise, and regular monitoring, it’s possible to keep blood sugar levels in check and reduce the risk of complications. Education, support, and staying informed about advancements in diabetes care are essential for anyone managing Type 1 diabetes.